Best Sleeping Position for Peripheral Artery Disease (PAD)
Peripheral Artery Disease (PAD) is a common circulatory issue where narrow arteries cause decreased blood circulation to the limbs. This situation can create a lot of discomfort, particularly during the night, affecting sleep quality drastically. Thus, finding the optimal sleeping position for Peripheral Artery Disease may ease discomfort and promote better sleep which benefits overall health and wellness. This article will explain PAD, its effects on sleep and how changing sleeping positions might ease the discomfort caused by it.
Understanding the Peripheral Artery Disease
What Causes Peripheral Artery Disease?
Peripheral Artery Disease (PAD) is a chronic circulatory disorder in which arteries become narrowed or blocked mainly in the legs from fatty deposit accumulation called atherosclerosis. This obstruction often causes leg pain, cramping, or fatigue, especially during physical activities. PAD might represent a far more extensive build up of fatty deposits in the arteries that, if untreated, may cause stroke and heart attack.
Common risk factors for PAD include:
- Aging
- Smoking
- Diabetes
- Obesity
- High blood pressure
- Cholesterol is high
Symptoms and Risks
Symptoms may include mild discomfort to severe pain that hinders daily activities and quality of life. They may experience claudication, leg numbness, coldness of the lower leg or foot, color change or slow-healing sores of the legs. Treatment for PAD generally requires lifestyle modifications, medication management to avoid blood clots or lower blood pressure and cholesterol, and in more serious cases, medical interventions to restore blood circulation. Early detection and adherence to a treatment plan may aid in the control of PAD and preventable complications.
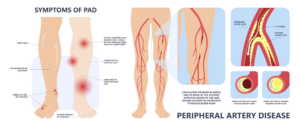
Main Symptoms:
- Leg pain/cramping
- Leg muscles fatigue/discomfort
- Claudication (pain during physical activity)
- Numbness or weakness of the legs
- Coldness of lower leg or foot
- Change of leg color
- Slow-healing sores or wounds on legs or feet
Sleep and its Role in the Management of PAD
Managing Peripheral Artery Disease (PAD) isn’t just about medical treatments and lifestyle changes; Sleep is important too. Good sleep allows the body to rest and repair, which is important for PAD patients. The body has various stages while you sleep, including stages for your physical and mental health. Notably, deep sleep stages allow for cell regeneration and repair, which is good for vascular health.
Sleep also affects the inflammation control and immune health that is important for PAD management. A well-rested body can resist inflammation, a key factor in PAD progression. Moreover, quality sleep helps with blood pressure and cholesterol regulation and may reduce PAD-associated risks. The interaction between good sleep and effective PAD management places sleep at the center of a holistic PAD management strategy.
Role of Restorative Sleep
Restorative sleep involves cycling through all the sleep stages including deep sleep and REM sleep. During these stages the body repairs and rejuvenates itself. For patients with PAD, restorative sleep may mean enhanced muscle recovery, improved mood and increased immune response. The pain and discomfort of PAD may be partially relieved by adequate rest and days of quality of life.
In addition, restorative sleep may improve cardiovascular health. Deep sleep also will cause your heart rate to slow and blood pressure to decrease, providing the heart and vascular system rest. This restorative process is essential for cardiovascular health and may retard the onset of PAD. Therefore, restorative sleep should be a goal for PAD patients as it promises better vascular health and better daily living.
Sleep Challenges in PAD
Sleeping with PAD could be tough because of the pain and leg pain related to this ailment. The intermittent claudication (pain from walking) may make sleeping a challenge at night. The pain may even wake people up from sleep, resulting in fragmented, non-restorative sleep. Poor sleep and increased pain may create a vicious cycle that affects well-being and the ability to manage PAD effectively.
Also people with PAD may have Restless Leg Syndrome (RLS), an ailment where the legs won’t move uncontrollably, especially at night. This condition may worsen sleep problems, causing insomnia or poor sleep quality. To overcome these sleep challenges requires a multifaceted approach. Finding the right sleeping position, controlling leg pain and addressing co-existing sleep disorders are important steps toward better sleep quality for PAD patients that may positively influence PAD management.
Sleeping Positions to Avoid after C-Section
Exploring Sleeping Positions for Maximum Comfort
Common Sleeping Positions
Everyone has different preferences in terms of sleeping positions. But a few sleeping positions are much better for patients suffering from Peripheral Artery Disease (PAD). Sleeping positions normally include supine position in the back (back position), vulnerable position on the belly (prone position) and side (lateral position). Each of these positions has particular characteristics and effects on body physiology.
The supine position is considered the neutral position, since the spine, head and neck are all in alignment, decreasing the likelihood of discomfort or pain. This position also allows for improved blood flow throughout the body – which is crucial for PAD. However, prone position is sometimes discouraged, especially in individuals with PAD, as it may prevent blood circulation and increase pressure on arteries. It might even cause discomfort in the neck and spine. The lateral position may be comfortable for many, and with proper support may also promote proper spinal alignment and circulation.
Advantages & Disadvantages
Each sleeping position has advantages and disadvantages, especially for PAD patients. The supine position maintains spinal alignment and promotes blood flow necessary for PAD management but can worsen snoring or sleep apnea. The prone position may be comfortable for some but can block blood circulation and strain the spine and arteries, making it less suitable for PAD patients. With support, the lateral position provides better circulation and less arterial stress, but can cause spinal misalignment and discomfort without support.
The choice of the right sleeping position is important for PAD management. It involves maintaining personal comfort while maintaining adequate blood circulation and lowering arterial pressure. Adjustments and supportive accessories such as pillows and mattresses may be necessary for better support and circulation.
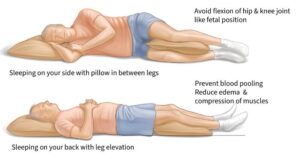
Best Position to Sleep for PAD
- Position of Elevated Legs
- Elevating the legs: Hovering the legs above the heart level may promote blood flow, reduce swelling and ease symptoms of PAD.
- With pillows or leg wedges: Supportive accessories such as pillows or leg wedges can be used to elevate the legs while sleeping.
- Adjustable bed: Investing in an adjustable bed can allow the legs to be raised to the desired height.
- Supine Position (Back Sleeping)
- Supporting spinal alignment: The supine position maintains a neutral spine for comfort and ease, and reduces additional arterial pressure.
- Better blood circulation: Lying on the back can provide better blood circulation than in other positions, which may be helpful in PAD management.
- Use of a supportive mattress: A supportive mattress can provide the support and comfort you need while back sleeping.
- Lateral Position (Side Sleeping)
- A decreased pressure on arteries: Side sleeping may relieve some of the pressure on the arteries which may be useful in PAD.
- Keeping the spine in alignment: Support with pillows between the knees can help maintain spinal alignment and comfort.
- Supportive mattress and pillows: Investing in a mattress and pillows that are supportive and comfortable may also help with side sleeping for PAD patients.
- Avoiding the Prone Position (Stomach Sleeping)
- Potential hindrance to blood circulation: The prone position can block blood flow and increase pressure on the spine and arteries, making it less suitable for PAD.
Other Beneficial Sleep Habits
Sleep-friendly Environment
Create an environment conducive to sleep is an essential process, particularly in the case of Peripheral Artery Disease (PAD) patients. Step one is picking a mattress and pillows that are supportive and fit the sleeping position. A well-chosen mattress can affect blood circulation and comfort while sleeping. Likewise, pillows can support the spine and maintain proper alignment of the spine to decrease artery pressure and promote blood circulation.
Cool, dark and quiet environment can also help with sleep quality. The recommended room temperature is 60 to sixty seven degrees Fahrenheit, as cooler temperatures are said to promote better sleep. Blackout curtains or eye masks can block out distracting light and earplugs or white noise machines can drown out noises. Also keep electronic devices away from the sleeping area to limit distractions and blue light that may disrupt the body’s sleep-wake cycle. Creating a clutter-free, relaxing environment may also promote better sleep and management of PAD symptoms.
Establishing a Regular Sleep Schedule
A normal sleep routine is crucial for PAD as it will help establish a predictable sleep-wake cycle which can enhance sleep quality. Heading to bed and waking at the exact same time each day (even on weekends) can help synchronize the body’s circadian rhythm which regulates the sleep-wake cycle. Developing such a routine sends a signal to the body that it is time to wind down and prepare for sleep and when you should awaken and get active.
Establishing a consistent bedtime and wake up time also can assist in settling into a sleep routine. Such rituals can include reading a book, going for a warm bath, practicing gentle yoga or meditation, or paying attention to music. Avoiding stimulants near bedtime and heavy meals and alcohol may also help with sleep. Setting up a routine to prepare the body and mind for sleep may enhance sleep quality, which is essential for controlling PAD and maintaining good health on the whole.
Consulting with Health Pros
Having professional consultations about managing PAD and optimal sleeping positions to relieve symptoms is important. Medical experts – particularly those focusing on heart health and sleep disorders – can offer individualized advice based on a person’s health condition and PAD severity. They can provide clues about how sleep positions may affect blood flow and suggest ways to improve sleep comfort and ease PAD symptoms. In addition, they may recommend additional therapies or interventions or even a sleep study to assess sleep quality and identify underlying sleep disorders that may worsen PAD symptoms.
Engaging with healthcare professionals also provides an opportunity to ask questions, voice concerns and learn about the link between sleep and PAD. They may offer educational materials, refer patients to other specialists such as sleep therapists or vascular surgeons for further evaluation and treatment, or suggest technological means such as apps and devices to monitor sleep and PAD symptoms. Open communication with and respect for healthcare professionals enables individuals with PAD to take a multidisciplinary approach to optimizing sleeping positions and environments for vascular health and wellness.




